Temporomandibular joint arthroscopy: inverted portal technique for more effective retrodiscal coblation
Abstract.
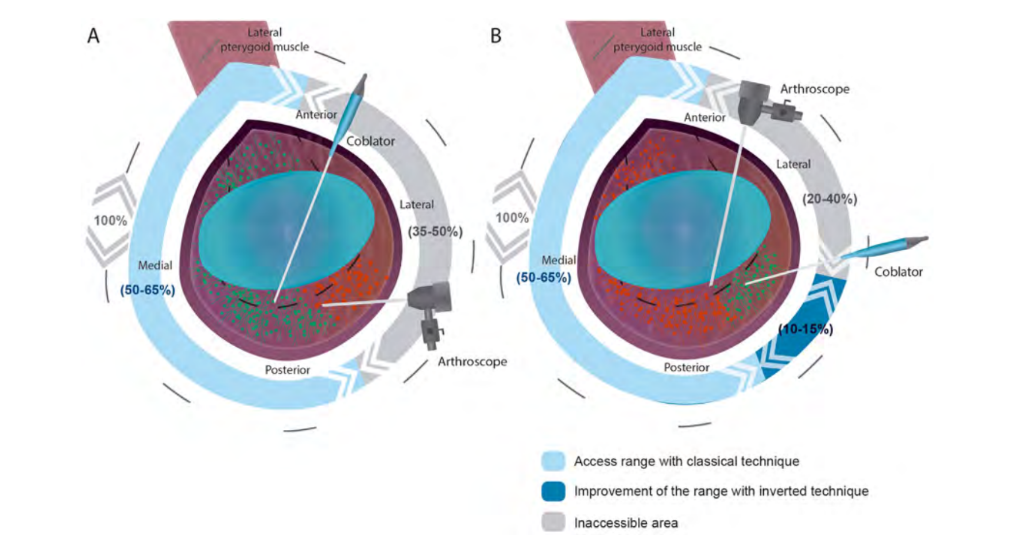
Temporomandibular joint (TMJ) retrodiscal tissue coblation is regularly performed as part of level 2 arthroscopy. It is usually performed with a coblator probe, which is introduced into the joint via an anterior working portal and visualized with an arthroscope connected to the posterior cannula. Coblation with the traditional landmarks is relatively easy in the medial, posterior, and anterior parts of the TMJ upper compartment; however, TMJ arthroscopy cannot access the entire upper compartment. Using the classical technique, it was estimated that surgeons can reach approximately 50–65% of the joint, and it is almost impossible to access the lateral and posterolateral areas. This technical note describes a simple and effective technique that improves access to the posterolateral area of the capsule for optimal retrodiscal coblation, increasing the treatment area by an estimated 10– 15% without the need for any additional puncture.
Coblation is regularly performed as part of level 2 and 3 temporomandibular joint (TMJ) arthroscopy to reduce inflammation and decrease the laxity of the retrodiscal tissue, as well as to facilitate capsulotomy or capsular release, synovial coagulation, chondroplasty, and fibrous debridement in the TMJ upper compartment. One of the main advantages of coblation, or ‘cold ablation’, is the precision debridement of damaged tissues at low temperatures (40–70◦C) without damaging the adjacent tissues.
The TMJ arthroscopic technique involving two portals has been well described by McCain et al., and represents one of the most common techniques for level 2 TMJ arthroscopy. The anterior portal, or working portal, allows the introduction of the coblation probe under direct arthroscopic visualization via the posterior portal. An important mission for the surgeon is to debride (remove inflamed or damaged tissues) the maximal area of the retrodiscal and synovial tissue. However, the triangulation angle obtained using this technique is suboptimal for accessing more posterolateral areas of the joint. Additionally, in the author’s experience, this angle is sometimes insufficient to coblate adequately the transition disc–retrodiscal zone. The purpose of this technical note is to describe a simple method to improve the coblation of the posterolateral retrodiscal zone (Fig. 1).
Technique
Upon completion of coblation treatment of the retrodiscal zone with the classical technique (Fig. 1), it is recommended that the coblator probe be carefully removed, followed by removal of the arthroscope while maintaining the cannulas in position with the aid of the assistant surgeon. With the portals in position, the arthroscope is placed in the anterior portal and a smooth probe is placed in the posterior cannula until direct observation is established. After obtaining direct arthroscopic control, the probe is removed and the coblator is introduced (Figs 1 and 2). The surgeon will now notice a new joint perspective. Untreated synovitis has often been observed in the posterolateral zone. The portal inversion technique increases the treatment area by an estimated 10– 15% (Fig. 1).
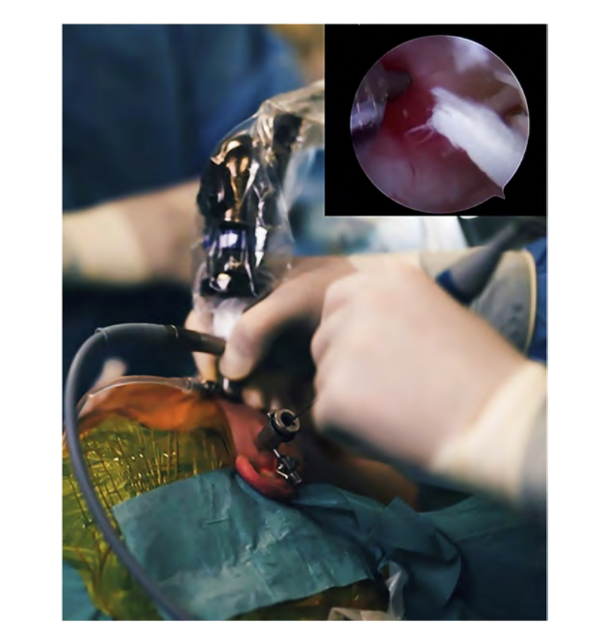
A 1.9-mm arthroscope with a 30◦ angle view, including a video system with a 2.8-mm outer protective cannula (Stryker, San Jose, CA, USA) was used. Coblation was performed using the ReFlex Ultra 45 Plasma Wand system (ArthroCare Corporation, Austin, TX, USA) with a 1.5 mm diameter. No attempt was made to perform more complex procedures such as disc repositioning with sutures. Note that both cannulas must be the same size. It is known that some surgeons use a smaller cannula for the working portal; in this case, the portal inversion will not be possible.
Discussion
Arthroscopic coblation is one of the most popular techniques in the orthopaedic field to effectively debride damaged tissues at low temperatures. Coblation is a more effective and safer method to debride tissue when compared to other systems. It is widely used in level 2 TMJ arthroscopy because of its wide variety of applications, including the following: to perform tissue debridement; to decrease the laxity of the retrodiscal tissue; to release the capsule/ anterior attachment of the disc and the attached lateral pterygoid muscle; to remove adhesions; to assist in chondroplasty; to perform synovitis coblation.
Fernández Sanromán et al. reported that TMJ arthroscopy using coblation technologies is a safe surgical procedure.
Regarding the localization of the debridement tissue, it has been reported that intra-articular adhesions mainly occur in the intermediate and lateral zones of the anterior compartment (approximately 20.8% and approximately 36.43%, respectively). The onset of adhesions can be a result of non-treated synovitis. Israel et al. described a strong relationship between arthroscopically diagnosed synovitis and adhesions (approximately 49% of the cases). In fact, the predominant localization of synovitis occurs in the posterior, medial, and lateral walls. In the author’s experience using the classical technique for TMJ arthroscopy described by McCain et al., most of the upper compartment zones are accessible, but not the postero-lateral and lateral zones. This limitation is due to the dead angle zone naturally created by accessing the joint via the lateral part. Considering a superior view and access to all walls of the upper compartment as 100%, the classical technique only allows visualization and access to approximately 50–65% of the joint (Fig. 1). The portal inversion technique was explored with the aim of increasing the visualization, and an increased range of visualization was observed. Recurrent untreated synovitis was most often observed in the posterolateral zone, with moderate to severe synovitis.
Currently, more than 50 joints have been treated with this technique, and the author is satisfied with the results, mostly because it is possible to extend the treatment area without the need for any additional puncture. A more ergonomic retrodiscal coblation with a ‘balancing movement’ of the coblator located in the posterior portal was felt, reinforcing the simplicity and effectiveness of this approach. It is considered possible to provide a better treatment for the patient with this refinement; however no rigorous data are available regarding the possible clinical impact of this modification.
In some patients, the author observed part of the lateral wall of the joint, with direct visualization of the entry point of the posterior cannula. The area surrounding the posterior entry point most often presents synovitis, but it is not possible to reach this zone with this approach. It was hypothesized that some TMJ arthroscopic failures could be related to untreated synovitis of the lateral zone of the joint, which is one limitation of TMJ arthroscopy. It would be interesting in the future to introduce a 70◦ angle arthroscope to learn more about the lateral part of the joint.
This technical note presents an improvement to the classical technique, increasing the access to the posterolateral part of the joint using an inverted technique (Figs 1 and 2). This improvement allowed the treatment area to be increased by approximately 10–15%, reaching a total of approximately 60–80% of the upper compartment of the TMJ, without the need for any additional puncture. This technique is only possible if the surgeon can perform the standard level 2 arthroscopy. Overall, the portal inversion technique is a safe surgical refinement, allowing for a new working vector and improving access to treatment zones.
References
- Kosy JD, Schranz PJ, Toms AD, Eyres KS, Mandalia VI. The use of radiofrequency energy for arthroscopic chondroplasty in the knee. Arthroscopy 2011;27:695–703.
- Chen YC, Lee SH, Saenz Y, Lehman NL. Histologic findings of disc, end plate and neural elements after coblation of nucleus pulposus: an experimental nucleoplasty study. Spine J 2003;3:466–70.
- Chen MJ, Yang C, Zhang SY, Cai XY. Use of coblation in arthroscopic surgery of the temporomandibular joint. J Oral Maxillofac Surg 2010;68:2085–91.
- McCain JP, de la Rua H, LeBlanc WG. Puncture technique and portals of entry for diagnostic and operative arthroscopy of the temporomandibular joint. Arthroscopy 1991;7:221–32.
- Anderson SR, Faucett SC, Flanigan DC, Gmabardella RA, Amin NH. The history of radiofrequency energy and coblation in arthroscopy: a current concepts review of its application in chondroplasty of the knee. J Exp Orthop 2019;6:1.
- Spahn G, Hofmann GO, von Engelhardt LV. Mechanical debridement versus radiofrequency in knee chondroplasty with concomitant medial meniscectomy: 10-year results from a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 2016;24: 1560–8.
- McFarland EG, Kim TK, Banchasuek P, McCarthy EF. Histologic evaluation of the shoulder capsule in normal shoulders, unstable shoulders, and after failed thermal capsulorrhaphy. Am J Sports Med 2002;30:636–42.
- Fernández Sanromán J, Costas López A, Fernández Ferro M, de Sánchez AL, Stavaru B, Arenaz Bua J. Complications of temporomandibular joint arthroscopy using two-portal coblation technologies: a prospective study of 475 procedures. J Craniomaxillofac Surg 2016;44:1221–5.
- Zhang S, Liu X, Yang C, Cai X, Chen M, Haddad MS, Yun B, Chen Z. Intra-articular adhesions of the temporomandibular joint: relation between arthroscopic findings and clinical symptoms. BMC Musculoskelet Discord 2009;10:70.
- Hakim MA, Christensen B, Ahn DY, McCain JP. Correlation of arthroscopic and histologic findings in synovial membrane disease of the temporomandibular joint. J Oral Maxillofac Surg 2020;78:1297–303.
- Israel HA, Langevin CJ, Singer MD, Behrman DA. The relationship between temporomandibular joint synovitis and adhesions: pathogenic mechanisms and clinical implications for surgical management. J Oral Maxillofac Surg 2006;64:1066–74.
- Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint: occurrence and location of osteoarthrosis and synovitis in a patient material. Int J Oral Maxillofac Surg 1988;17:36–40.
/social-network-service/media/default/6809/fbab08d0.jpg)